
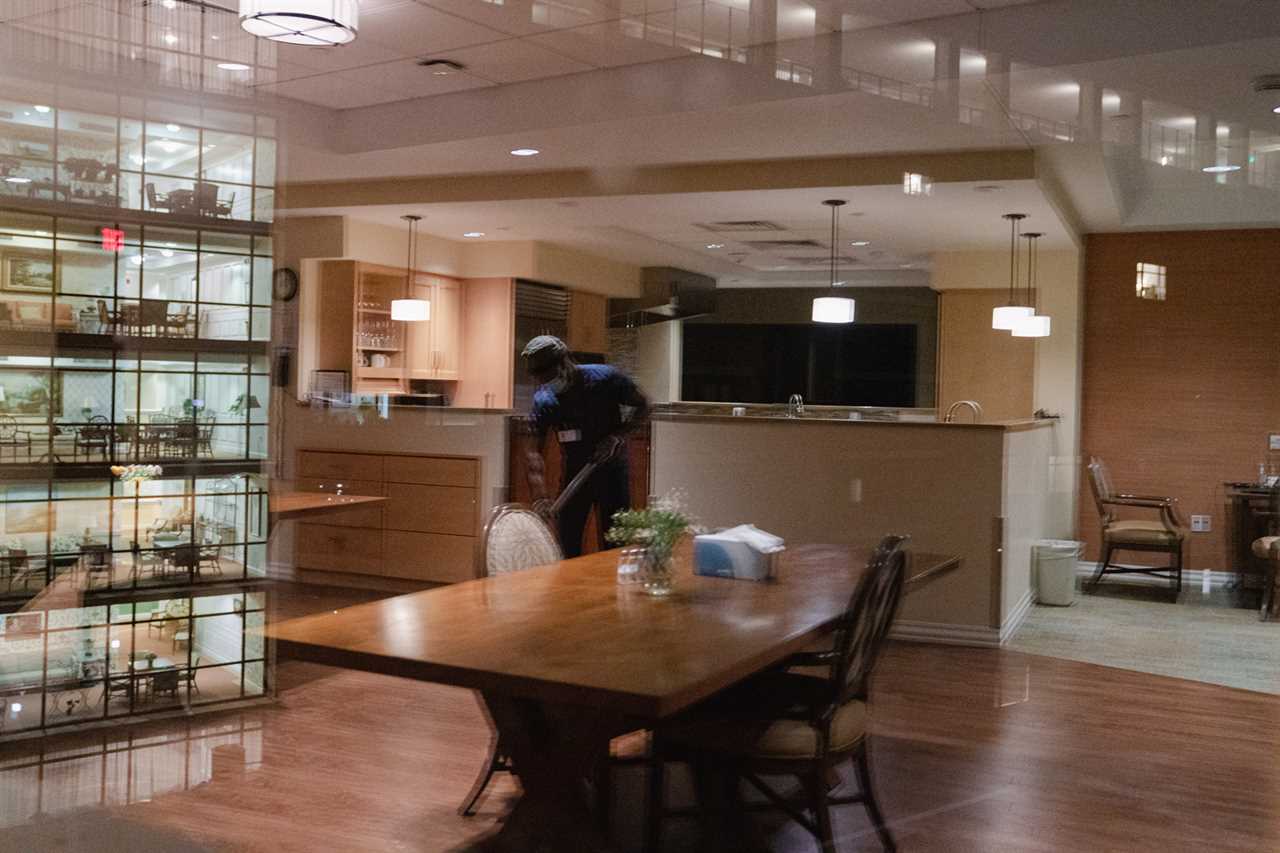
December blurred to January, and the night shift blurred into the day shift, as Momah Wolapaye, 53, rotated warm towels beneath the bedridden at the nursing care wing for the Covid-positive. Repositioning the residents every two hours prevented bed sores, and normally took two aides, but now only one was permitted in rooms. Straws were also forbidden, so after giving sponge baths, Wolapaye spoon-fed sips of water to the elderly, checked their breathing and skin coloration, and calmed the anxious who called into the night silence.
Most didn’t understand why they were suddenly in new rooms, sealed with painter’s plastic, and why they needed masks. Some wanted to leave, and Wolapaye spent 20 of the 30 minutes inside each room calming them and explaining “the virus.” It was December 2020, the pandemic’s second wave, and all but three staff on his team had caught Covid. His supervisor asked if he could work 16-hour shifts. He agreed. He tied his blue uniform in a plastic bag when he got home in the morning, told his sons not to touch it, and returned to work that evening to Goodwin Living, a long-term care community in D.C.’s suburbs.
Wolapaye stands out: He genuinely loves his job, one known for burnout, mistreatment and injury. “It’s my responsibility, being there with the residents. I take them to be like my own people.”
Since January 2020, 400,000 nursing home and assisted living staff have quit, citing pandemic exhaustion as well as the low pay and lack of advancement opportunities typical of the field. The job losses arrive when America already faces an elder caregiver shortage, as 10,000 people daily turn 65 and birth rates decline. The labor shortage gripping America’s workforce across industries is felt most acutely in home health care. According to the Bureau of Labor Statistics, home health and personal care aides are actually the fastest growing industry, projected to grow 33 percent in the next decade, much faster than all occupations. But there still simply aren’t enough workers to fill the demand.
“The numbers alone suggest we’re going to need a lot more people in the caregiving sector than we have now,” says Tara Watson, a fellow at the Brookings Institution and professor of economics at Williams College. “We need to make some changes in order for that to happen.”
For decades, elder care in the U.S. has been bolstered by an immigrant workforce. As a new immigrant from Liberia, Wolapaye found his first job in America at Goodwin Living 11 years ago. Immigrants occupy nearly 70 percent of jobs at the Alexandria, Va., facility, and are 40 percent of home health aides. But today, international migration to the U.S. is at record-lows. And with native-born Americans apparently reluctant to take elder care jobs, economists like Watson are raising alarm bells: Who will care for America’s elderly?
It’s a particularly important question as the crisis we’re in now is nothing compared to what’s coming: The percentage of people over the age of 85 — the group that most needs care — is predicted to double to 14 million by 2040, in part because Americans are living longer. In 2050, 84 million elderly people will live in America. Virginia alone is projected to be short 23,000 nurses in the next decade.
“The demand for this isn’t going to go away because the demand is being driven by an aging population,” says Dan Kosten, assistant vice president of policy and advocacy at the National Immigration Forum.
Still, despite the challenges that have pushed so many away from elder care work, immigrants, like Wolapaye, continue to seek and have remained in these difficult jobs. Wolapaye has stayed at Goodwin Living and — with good pay, benefits and advancement opportunities — has no plans to leave. His favorite residents are the ones who are quick with a story, like one resident nicknamed (for his time in the U.S. Army) General. Goodwin Living has been home to hundreds of retired government officials, including CIA agents, Navy admirals, and, at one time, former National Security Advisor Brent Scowcroft and former President Ronald Reagan’s press secretary, Jim Brady. (Disclosure: My mother-in-law also lived there, before dying of Covid.)

The story of Wolapaye’s path to the U.S. and Goodwin Living — and his decision to stay in the industry — offers a roadmap for policymakers to address the elder care crisis in America. Ultimately, broad immigration reform, as well as a comprehensive policy push at the state and federal level for better pay and working conditions in the caregiving industry, is required.
It was 2010, Sociology 400 was his last exam, and Wolapaye was walking a 90-minute commute to take it, at the University of Liberia, when his Nokia phone rang: He had been selected for a Diversity Visa, better known as the “The Green Card Lottery.” He stopped in the road, in disbelief. He had filled out a lottery form with 13 million other people that year but hadn’t expected to win. Things had not been easy. Liberia’s Civil War shut down his high school for 15 years, and he passed the time volunteering at a war-wrecked hospital. One brother died by Gaboon viper, another by motorcycle accident. Recently he had become a father and needed to provide for his family. This was his “golden ticket,” he said.
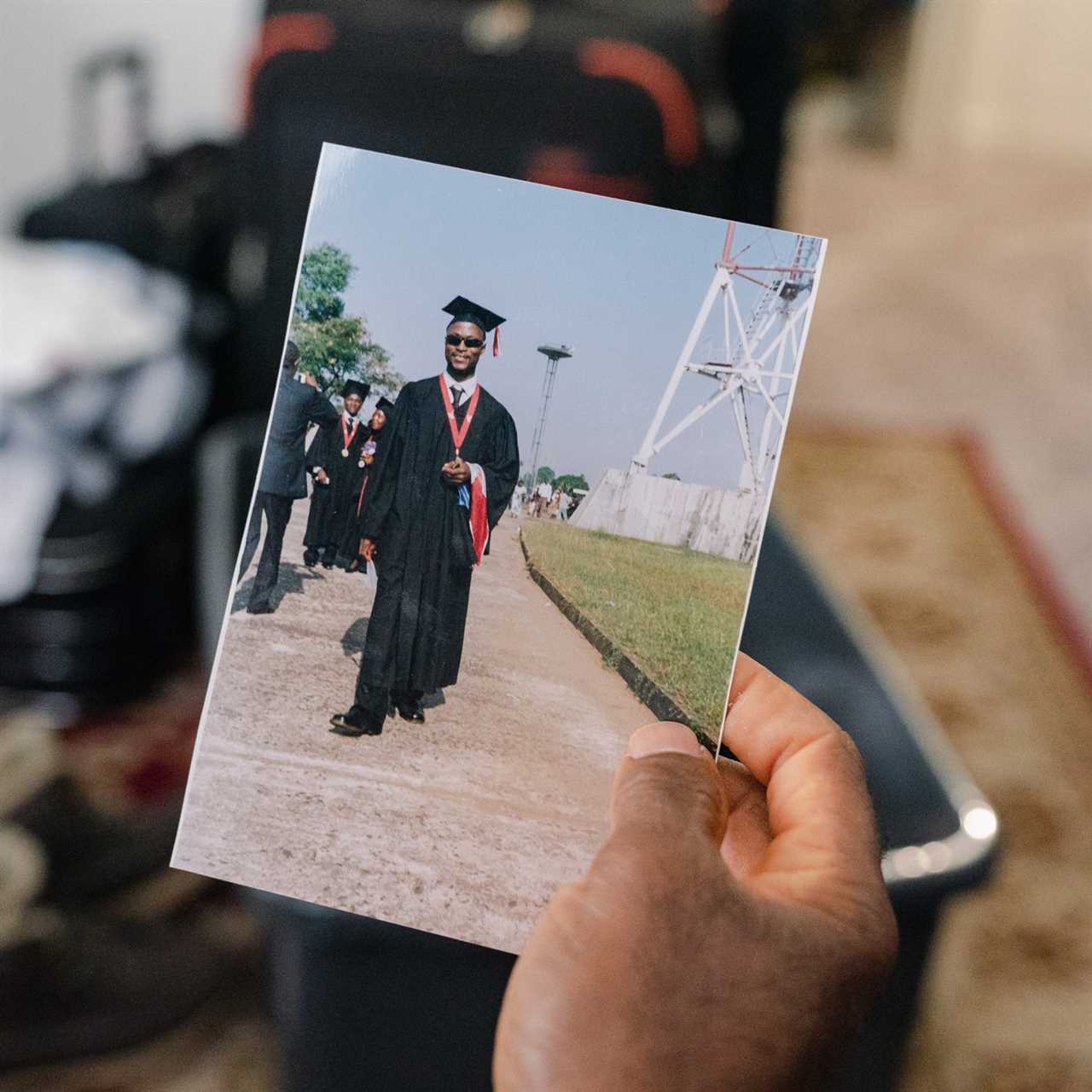
When Wolapaye won the Green Card Lottery, he knew no one in America, but a friend had a friend he could crash with in a place called Virginia, so he set forth from Bong County, in Liberia’s north, to the friend of the friend’s apartment in Alexandria. Four weeks later, a job posting on Google caught his eye: A long-term care facility, up Beauregard Street, needed a food prep assistant.
Wolapaye says he was raised to revere elderly people, and he had cared for his own father before he died. He got the job. Chopping vegetables in the back kitchen soon led to a promotion, after 120 training hours, to Certified Nursing Assistant. CNA jobs, and caregiving generally, are considered low-barrier — a quick route to a paycheck, particularly for new immigrants looking for work. And elder care is bursting with work. But America’s immigration policies have not kept pace with its aging demographics, and the country faces a caregiver shortage, with many experts arguing that it’s already here.
When Wolapaye emigrated 10 years ago, 50,000 Diversity Visas were awarded annually. His golden ticket would be nearly impossible today: 18,000 Diversity Visas were awarded last year, with 3,000 forecast for this year. Net migration to the U.S. has plummeted from 1 million in 2016 to 250,000 in 2021. The decline — from pandemic restrictions, shuttered consulates, backlogged visas, Trump immigration policies and changes in global migration — will right itself slightly as the pandemic lifts, says Watson, but not to 2016 levels.
With fewer immigrants coming, elder care work goes unfilled.

“New immigrants take the care jobs,” says Jeanne Batalova, senior policy analyst at Migration Policy Institute. Many long-term care workers are from countries where English is the official language or taught in school, like the Philippines. Over a third are from the Caribbean or Africa. English skills make it easy to get a job as a nursing assistant, for which no other skills are often required. Although some have a background in health care, they’re considered low-skilled workers, because degrees and proficiency are not needed.
But low barrier to entry shouldn’t be confused with low-skilled, says Pat Armstrong, a Canadian sociologist who spent 10 years studying nursing homes in the U.S., U.K., Canada, Germany, Sweden and Norway.
“You have someone with dementia who you’re trying to get to eat. It’s not so easy. Someone sits there and says, ‘Nurse! Nurse! Nurse!’ repeatedly for 10 hours. You realize how incredible they are to go back there, day after day.”
Elder care requires significant “people care” skills, says Steffie Woolhandler, professor at CUNY School of Public Health at Hunter College. In a study of Filipina elder care workers in Los Angeles, the majority cited “companionship” as their top job responsibility, over “Activities of Daily Living” like bathing and feeding. A companion is a surrogate family member — news-provider, anxiety-reducer, FaceTime operating system-fixer, an eyes and ears to daily life. Their presence relieves loneliness and depression, as lethal as other chronic health conditions, says the study’s author, Jennifer Nazareno, assistant professor at Brown University School of Public Health. Companions alleviate the financial burden on the health care system from falls and hospitalizations.
But these roles and jobs have not been valued by immigration or labor policy up to now. The preference is towards “high-skilled” workers, like programmers and doctors. “Once you talk about a level of skills for home health, it’s as if there’s an aversion,” says Kosten, who suggests that what’s really needed is a new category of low-skilled employment-based visas.
Can’t these jobs be filled by American-born workers?
They don’t want them. The pay is too low, will likely never be high, and the American workforce has become more educated with bachelor’s and master’s degrees. Elder care jobs, if they get filled at all, Kosten says, will go the way of agriculture jobs — now 70 percent filled by immigrants — but only if policymakers make it possible.
But even if native-born workers took the jobs, we’d still have a shortage, say economists like Watson. In 2040, the demographics across America will resemble the oldest parts of Florida today. “There simply aren’t enough American workers to support the growing elderly population that we have,” to counter the millions leaving the workforce, not being replaced and needing care.
Perhaps the biggest problem is that workforce shortages facing elder care is an issue most just don’t see. If you don’t have enough construction workers, you see a half-built building, says Batalova. But while the elder-care crisis is behind closed doors, it will be one of the most acute issues in about five years, she says. And, to prevent that, “immigration is one of the policy tools that policy makers should start working on.”
For a glimpse at the United States’ future, check out Japan, which is one of the fastest-aging societies in the world. Automation first seemed promising for elder care, until serious challenges emerged: If a robot lifted someone whose leg was injured, it could pinch them or inflict pain but lacked “sensory perception” to detect it. Despite a historic resistance to immigration, Japan’s parliament passed a measure allowing hundreds of thousands of immigrants into the country in 2018 to address labor shortages including for elder care.
The lesson of Japan is, “‘I don’t want a robot,’” says Batalova. “‘I want a human touch.’”
Wolapaye agrees, recalling General announcing to his smart speaker, “Hey, Alexa, what’s the news?” Alexa could rattle off the headlines but couldn’t have the kinds of conversations with General that Wolapaye did, like listening to him reminisce about the country music festivals he enjoyed after retirement and laughing with him as General danced in his wheelchair to country music. He asked Wolapaye when his children were arriving from Liberia and said he wished to meet them.

General and his wife lived in separate rooms but insisted on kissing before bed each night. The staff would direct a wheelchair choreography: Wolapaye wheeled General over, lifting him to stand, while another aide lifted his wife to her feet. They’d kiss, and the staff would clap, before the couple returned to their rooms.
One winter morning late in December 2020, Wolapaye got off the night shift, returned to work that evening and saw the first three rooms of Shenandoah House — the health care wing, named for the Virginia river — sealed with floor-to-ceiling plastic. Three residents were infected, which soon grew to eight, including General.
When the virus came for Goodwin Living, ‘Who will care for America’s elderly?’ was suddenly not an abstract policy question but an immediate, practical one. Shenandoah House was separated into the “Warm Zone” for Covid-exposed residents and the “Hot Zone” for Covid-positive. Painter’s plastic cordoned off the common kitchen, but disease jumped down the hallway; Warm became Hot, and the staff working both zones became infected.
Wolapaye said, “Put me in the Hot Zone,” and began 16-hour shifts for three-to-four-day periods.
“This is what I signed up for, as a Certified Nursing Assistant,” he said. “Someone has to take responsibility and risk their life.”

Working 16 hours straight is not uncommon for long-term care aides, says Nazareno, citing the average shift of care workers in her study at 16.6 hours. But putting in this kind of labor must come with basic protections, like a living wage, health insurance and a path to citizenship, she says. After all, why not work at Amazon, which at least comes with health benefits?
Finding more workers to do these jobs is only half the solution: Higher pay and opportunities for career advancement are critical for retention. In fact, the root of what plagues the long-term care industry is not a worker shortage but a wage shortage, says Charlene Harrington, professor emerita of sociology and nursing at UC San Francisco. Most direct care aides are paid on par with fast food restaurants, at $13- $15/hour, and live below the federal poverty line. Many lack health insurance. The workloads are too heavy — a CNA should be responsible for seven residents, but many are responsible for 12 or even as many as 25, says Harrington. Burnout creates turnover, as employees depart for fast-food and housekeeping jobs with similar wages but fewer stressors, she says. And it’s not just up to the industry to self-correct. The government can play an important role in instigating changes.
Earlier this year, the Biden administration proposed a slate of executive reforms that could help. The new measures call for increased oversight of nursing home ownership, financial transparency and minimum staffing standards — found to be low in almost every state. “Seventy-five percent of all nursing homes have inadequate staffing,” says Harrington, an “appalling” reality that research has shown for 20 years but which the pandemic made obvious. She notes that lower RN staffing led to increased nursing home Covid infection and deaths. Harrington is glad some action is taking place at the federal level, but more needs to be done, she says, and she finds some of the most promising initiatives coming from states, which have more room to regulate how a nursing home spends its money.
Several states like New York, New Jersey and Massachusetts have set “direct care ratios,” which ensure a limit on profits so that more expenditures are directed to care, in an industry where 70 percent of nursing homes are for-profit. Since the onset of the pandemic, five states have adopted permanent increases to nursing home staffing requirements, and four have adopted laws or regulations for increased nursing home wages. “The nursing homes need to step up and start paying decent wages, and I don’t think they’re going to do that until they’re required to do it,” says Harrington. “You can’t have a decent, stable workforce unless you increase the wages and benefits.” And even so, all these changes relate to nursing homes, which represents only a fraction of all elder care; of 14 million elderly adults currently receiving some form of care, approximately 1 million are in nursing homes.
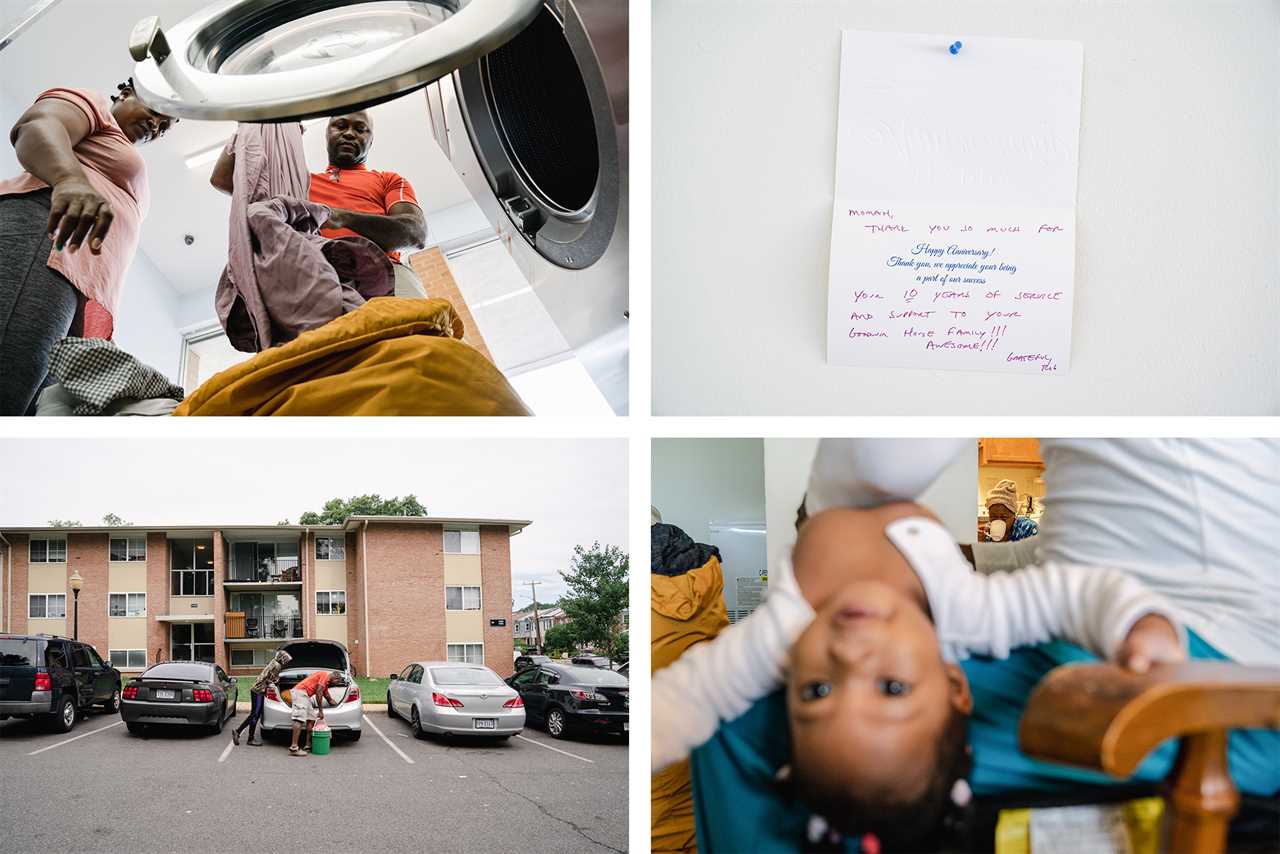
Wolapaye earns more than most nursing assistants, at $20.50 per hour, with medical, dental and life insurance, a 401(k) and paid time off. Tuition assistance is provided for up-training. And the facility covers the $750 U.S. citizenship application fee for employees who have worked six months or longer, arguing it helps retain workers.

Lack of advancement is another reason many CNAs quit. Wolapaye followed a ladder: Dining Assistant led to Certified Nursing Assistant; then he earned a Med Tech certificate; then he began school to become a Licensed Practical Nurse, until his brother died, who was looking after his kids in Liberia. Wolapaye took on double shifts to pay for their education. His goal remains: Registered Nurse, who average $39 per hour in the U.S. His path to get there has been long and arduous, even as he’s had more advancement opportunity than many elder care workers.
Helping establish career ladders is one way federal and state governments can assist providers in retaining workers, says David Grabowski, professor of health care policy at Harvard Medical School. Providers like Goodwin Living are equipped to do this, in part, from private pay. But for others, like small providers who make up the majority of assisted living communities, he says the government should create roadmaps for partnering with community colleges that offer training programs, or incentives, or loan forgiveness for workers. “If cost is a big barrier here, which it is for many individuals in this workforce, we should completely invest in making [advancement training programs] free.”
The hardest position for providers to fill is often Registered Nurse. When a worker ascends from a nursing assistant to a nurse, it’s a “win-win,” says Grabowski, because the provider fills a role they need and the worker gains economic mobility. “Staffing shortages are taking up all the oxygen right now in the room in long-care,” he says, citing a “desperation” among providers, who are competing with each other for staff, with some offering ownership stakes and signing bonuses to new direct care workers. “Allowing someone to climb a career ladder” is a much better, more sustainable path, he says.
If there are no policy changes, America will be a country where its seniors do not live or die with dignity, says Woolhandler. The quality of care will deteriorate: fewer baths, fewer people to prepare food or help with toileting. An understaffed, demoralized workforce leads to more disease transmission, she notes. More seniors will be bedridden; there will be more falls, when people do try to move about, with some discovered days later.
As Wolapaye continued working the Hot Zone, General’s symptoms worsened, and he was sent to the hospital. Soon afterwards, Wolapaye called General’s wife to check on her. She was a night owl, surfing TV channels, and they’d developed a friendship. He raised the bed head to make her comfortable. The next day, he knocked on her door, and she tried to turn her head in his direction. He reported to the nurse that something was wrong. The next evening, she was sent to the hospital.
As the virus worsened, some staff at Goodwin Living declined to work, and those who did come in avoided Wolapaye and the others tending to the Hot Zone. They were trying to keep their families healthy and alive. But Wolapaye was trying to keep his family alive, too — that included General and his wife. “They were like my father and mother,” he told me.

Nine days before vaccines arrived at the facility, General died, and 13 days later, his wife died, as well as two others from the Shenandoah Hot Zone. It was a tragedy for everyone, and Wolapaye could have taken time off to grieve, but he felt he had to be there, to continue taking care of others.
Today, Goodwin Living no longer cordons off a Hot Zone, but the elder care industry, and health care generally, finds itself in a Hot Zone of another kind: nursing scarcity.
Sitting with his family outside his apartment complex, on a sweltering July afternoon, Wolapaye considered his future in America. “In five years, I want to be a Registered Nurse,” he said, ready as ever to be a part of the solution.
----------------------------------------
By: Alexandra Moe
Title: Who Will Care for America’s Elderly?
Sourced From: www.politico.com/news/magazine/2022/07/28/elder-care-worker-shortage-immigration-crisis-00047454
Published Date: Thu, 28 Jul 2022 03:30:00 EST






