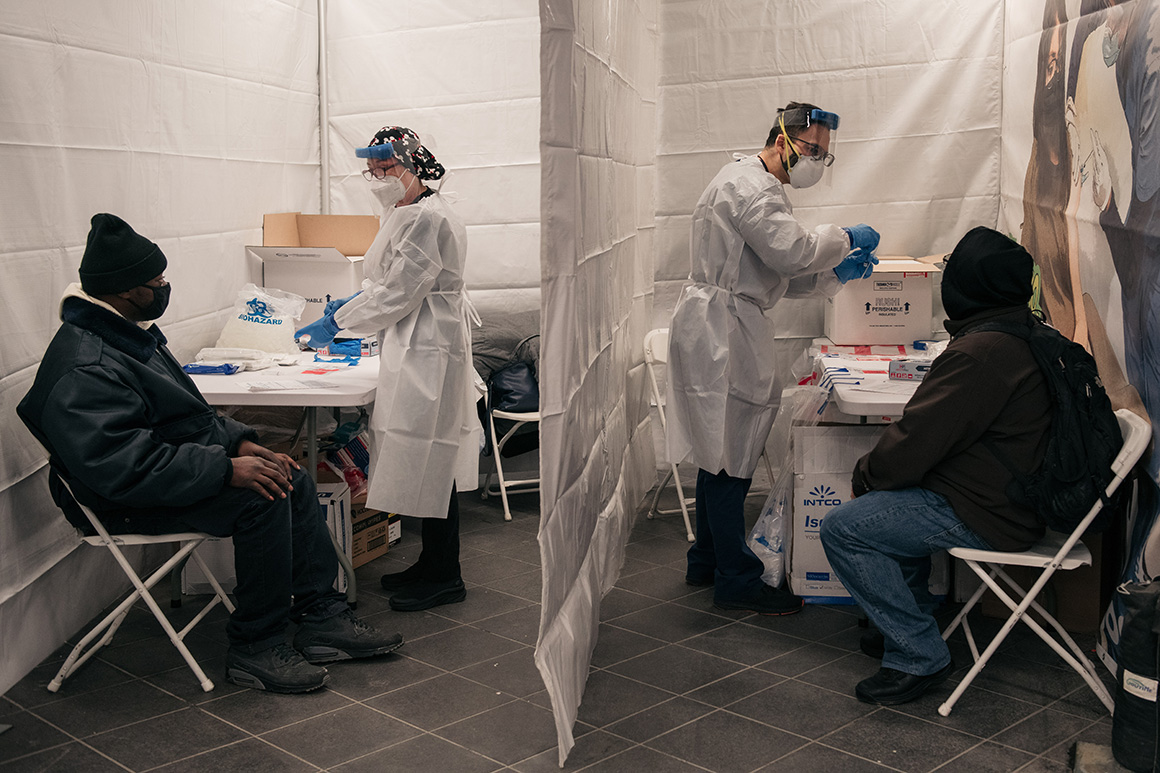
Testing laboratories at the center of efforts to track the spread of Covid-19 expect to face record demand in the coming weeks while their workforces are depleted by the very virus they’re surveying.
Public health experts and testing company executives are concerned the surging Omicron variant could upend efforts to use Covid-19 testing to keep schools open, treat patients and make public gatherings safer.
The Biden administration is relying on testing to keep the country going and help avoid a return to stricter public health restrictions. But there may not be enough workers to process an avalanche of tests. Vault Health CEO Jason Feldman, whose company runs Covid testing programs, said that about 40 percent of the staff at one of the company’s Northeast labs recently got sick, stretching the time it takes to turn around results.
“I think what's going to happen is as this thing moves across the big population states like Texas and California the s--- is going to really hit the fan because there's just not enough capacity of people, lab techs to keep these labs going,” Feldman said.
While the supply chain for once-scarce equipment like test kits and pipette tips remains intact, the sheer demand for testing is stretching sample collection sites and laboratory staff. One pharmacy industry source told POLITICO that lab staffing issues are already limiting testing capacity and turnaround times for testing done through major retail chains.
“The question is how well do they keep pace,” said Céline Gounder, an infectious disease specialist who advised the Biden transition’s Covid-19 response. “If you get to the point where — as we've seen in some cities — lines are hours long to get a PCR test and you go to every retail pharmacy in your neighborhood and they're all sold out of rapid antigen tests, at some point people will give up and say it's just trouble. It's not worth it.”
The U.S. is recording more than 2 million test results per day, a record high, according to a tracker maintained by Johns Hopkins University. But public health experts caution that number is missing millions of at-home test results due to widespread underreporting by the public and inconsistent data collection by public health departments across the country. CDC data shows shows more than 554,000 Covid-19 infections are being recorded each day — a number experts believe is a significant undercount.
The White House is “actively tracking the issue of staffing shortages and currently exploring ways we can assist,” a senior administration official told POLITICO.
To get more of a real-time picture, labs may have to surge their workforces and add shifts. But that could prove difficult with so many technicians falling ill.
“We haven't had anything hit in the lab specifically yet where we've had to do any kind of emergency staffing,” Mayo Clinic Laboratories President William Morice said. “But overall for the health system we’re definitely seeing the number of employees who are testing positive really going up.”
Quest Diagnostics on Tuesday said its turnaround time is now two to three days on average, up from one day in late December due to an Omicron-driven surge in testing demand. Rival Labcorp said its average turnaround for PCR test results is still at one to two days.
“I think the staffing is a rate limiting factor for laboratories of all kinds,” Association of Public Health Laboratories CEO Scott Becker said. “It's not like the Biden administration can just use the [Defense Production Act] for people.”
Another potential bottleneck in the weeks ahead is the number of collection sites where people can get tested — an issue the Biden administration is trying to remedy by expanding the number of sample collection sites.
“Additional sites are opening this week in Washington, D.C., Philadelphia, with Maine, Maryland, Nevada, Delaware, Texas and Washington state to follow,” White House Press Secretary Jen Psaki told reporters on Wednesday.
Testing company Curative has had to cap the number of testing appointments it offers and even close some of its collection sites temporarily because of widespread infections among staff, according to spokesperson Miranda Gottlieb.
“We still metered some appointments to be able to maintain turnaround times last year, but we did not have to shut down early or close a site because of staff being ill,” Gottlieb said.
Obstacles that beset Covid-19 testing earlier in the pandemic, like shortages of pipette tips and reagents necessary for scaling up lab-based testing, are now under control, Qiagen CEO Thierry Bernard told POLITICO.
“HHS in the U.S. is having scenarios by which this could move up to above 2 million PCR tests per day needed in January — they even say that at a point between two to four,” Bernard said.
“We can probably swallow the increase of tests that HHS is modeling.”
Mara Aspinall, an adviser to the Rockefeller Foundation and member of OraSure Technologies’ board of directors, agreed that the supply chain for labs has benefited from extensive government investment, but noted lab staff are dealing with more than Covid test volumes.
“People are going back to doctors’ offices,” Aspinall said. “They're having biopsies and mammograms and physicals and blood tests. So the challenge that the labs have today is they have an enormous number of Covid tests. But in addition, they have general tests that they didn't have a year ago when so many doctors' offices were closed.”
Arvind Kothandaraman, managing director of specialty diagnostics at PerkinElmer, said turnaround times at labs using the company’s instruments and reagents are still around one day, but noted that some are seeing a five-fold increase in positivity rate alongside a doubling in sample volume.
“If the testing volume follows the positivity rate trend, then we may have some trouble down the line,” Kothandaraman said. “Not knowing when Covid is going to go away, it just makes it all the more difficult for them to hire staff and retain staff. That’s been the primary challenge.”
High positivity rates pose a particular challenge for schools and workplace screening programs that utilize pooling strategies — in which samples from multiple individuals are tested at the same time. When a pool tests positive, individual samples need to be evaluated. And too many positive pools drives up demand for tests and can increase wait times.
Georges Benjamin, executive director of the American Public Health Association, argued the U.S. needs to figure out how to best use its testing capacity as Omicron cases overtake more of the country.
“We need to sit down and rationalize how we're using tests and try to figure out how we prioritize them so we have a rational system so that people aren’t doing testing in ways that don’t necessarily help with our productivity and our ability to engage society,” Benjamin said.
----------------------------------------
By: David Lim
Title: They need to process your Covid tests. Now they’re out sick from Omicron.
Sourced From: www.politico.com/news/2022/01/07/covid-testing-staff-shortage-526701
Published Date: Fri, 07 Jan 2022 04:30:19 EST






