From racial bias in CPR to private equity price hikes, here’s what researchers learned about US health care this year.
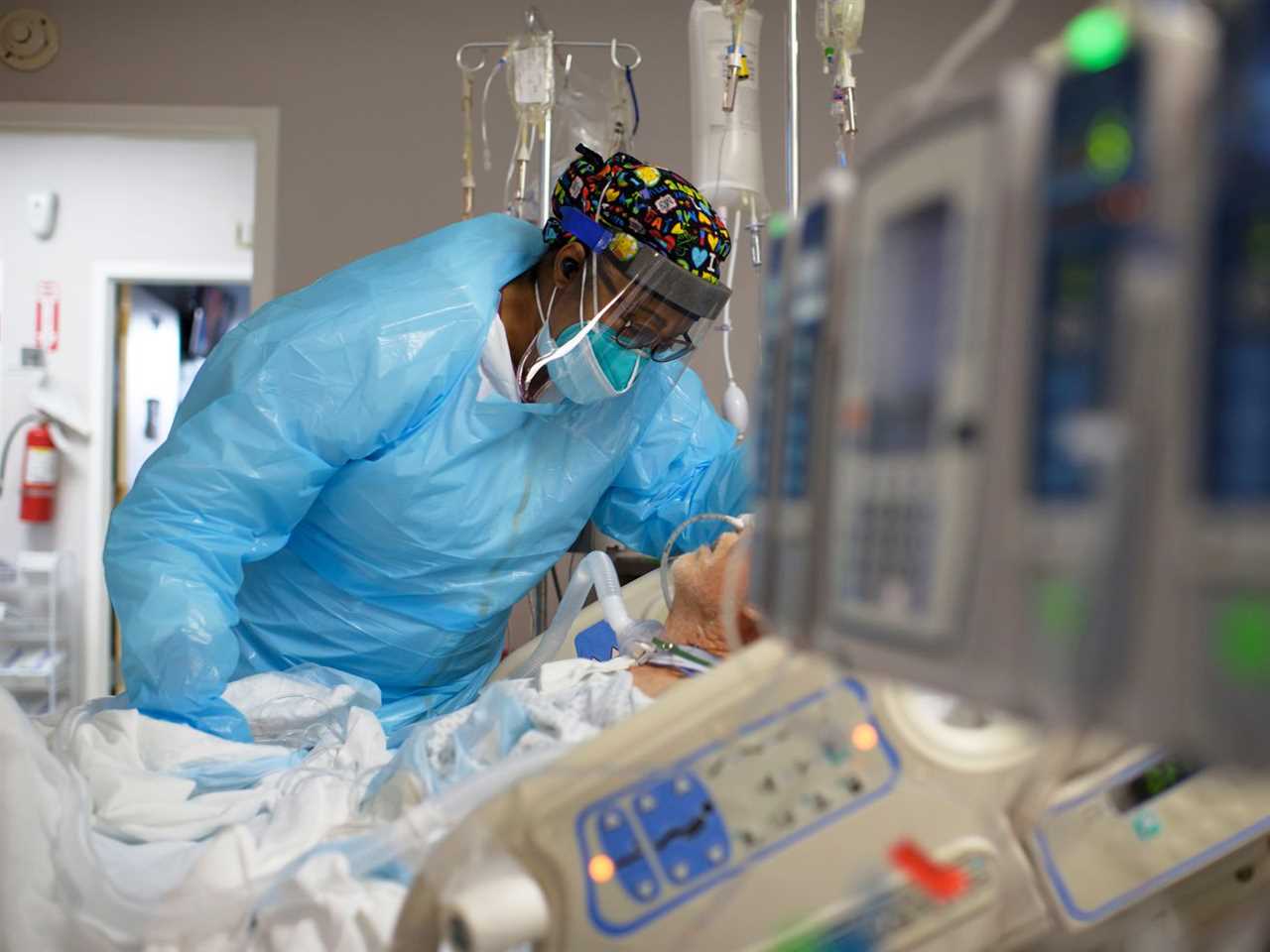
Though the pandemic and all its attendant health care crises remained the major health care story of 2022, churning all the while in the background has been the critical work of academic scholars, operating on longer timelines, who are still trying to make sense of US health care and of medicine itself, to get a better idea of what’s wrong and how to make it better.
To wrap up this year, I asked a couple dozen health policy experts what research released this year (though, as one of them reminded me, these papers are often years in the making) had surprised them, changed their thinking, or struck them as especially notable.
Here are five particularly interesting papers, at least in my view. Because many more than that warrant mention, I have tried to cram in as many references to other work as I could. One of my lessons from this exercise was that there are noteworthy new studies being produced all the time. The US health system certainly merits such extensive investigation, given the number and diversity of its flaws.
These studies cover a broad range of subjects, from the intricacies of Medicaid provider networks to prescription uptake by Medicare beneficiaries to how bystanders react when a person experiences a cardiac episode in public. But first, on the topic of the pandemic...
1) Vaccination education campaigns in nursing homes didn’t make much difference
Several experts pointed me to data sets related to Covid-19 vaccination in nursing homes, the scenes of so much illness and death in that frightening first year of the pandemic. Larry Levitt, executive vice president of the Kaiser Family Foundation, flagged one recent KFF survey that found less than half of nursing-home residents are up to date on their vaccines.
That put into sharp relief the findings of a study that Harvard Medical School’s David Grabowski cited as one of his favorites of the year. The paper, published in JAMA Internal Medicine in January 2022, evaluated an effort to use educational campaigns and other incentives to improve vaccination rates among residents and staff in nursing homes.
They did not find a meaningful effect, despite three months of programming. There was plenty of room to grow, particularly among the staff, roughly half of whom were unvaccinated during the study period. (Vaccination rates among residents were already high at the time, though the experiment still did not find a significant effect of the multi-faceted campaign.)
“The conventional wisdom was that a big part of lagging vaccination rates was a lack of information and knowledge about the benefits of vaccination,” Grabowski said. But this study found instead that “these educational efforts were unsuccessful at encouraging greater vaccination. Although information campaigns sound like great policy, they really aren’t.”
He lamented that the study had been ignored by policymakers, noting federal efforts to increase vaccination rates among this population remain focused on education. Grabowski said the policies with the strongest evidence are vaccine clinics and vaccine mandates for staff.
2) Medicaid’s “phantom” networks may overstate patients’ access to health care
I love good jargon, and “ghost physicians” is one of my favorite new phrases of the year, which was recently brought to my attention by Harvard University professor (and former Vox contributor) Adrianna McIntyre.
It comes from this May 2022 Health Affairs paper, authored by Yale University’s Avital Ludomirsky and colleagues, which evaluated the provider networks of Medicaid managed-care plans. Those are privately administrated plans for low-income people that must follow state and federal Medicaid rules; they have grown in enrollment in recent years, with more states deciding to outsource their role in providing health coverage for the most vulnerable.
One of those rules is that enough doctors and hospitals accept those Medicaid plans, otherwise known as network adequacy. The Health Affairs study examined managed-care plans in four states over several years to get a better sense of providers’ participation in the program.
Their most striking finding is that while nominal participation was fairly high, about one-third of providers who technically accepted Medicaid actually saw less than 10 Medicaid beneficiaries in a given year. The responsibility for providing care to these patients was concentrated among a small number of practices, with 25 percent of primary care doctors providing 86 percent of the care and 25 percent of specialists providing 75 percent of those services.
In other words, while plenty of doctors might say they accept the plans, people who are enrolled in them may in practice find they have relatively few doctors to choose from. “Our findings suggest that current network adequacy standards might not reflect actual access,” the authors wrote in their conclusion. “New methods are needed that account for beneficiaries’ preferences and physicians’ willingness to serve Medicaid patients.”
The move toward more Medicaid-managed care has spurred a lot of debate and study. Matthew Fiedler, senior fellow at the Brooking Institution, sent me a Harvard study with its own surprising finding: In Texas, transitioning Medicaid enrollees to managed care had actually led to an increase in the use of prescription drugs and outpatient services, while the number of avoidable hospitalizations fell.
What seems to have happened, Fiedler said, is the state had been “penny-wise, pound-foolish” when running the program itself by imposing an unusually strict cap on the number of prescriptions patients could fill in a year. With that cap relaxed under the managed-care plans, patients filled more prescriptions and that corresponded to fewer episodes in which they ended up in the hospital when they didn’t have to.
Fiedler thought the study could also have implications for Medicare Advantage as well, another version of a government health insurance program that is being administered by private companies.
“To be clear, in many of these cases, it might well be better to fix this problem by just fixing the public program directly,” he told me. “But given that we often seem unwilling to do that, this does point to one very real advantage of involvement from private plans.”
3) Many Medicare beneficiaries don’t fill important prescriptions
Rachel Sachs, who studies prescription drug policy at Washington University in St. Louis, highlighted a study on a similar subject that was published in Health Affairs in April 2022, led by Vanderbilt University’s Stacie Dusetzina. The researchers studied the difference in prescription uptake by Medicare beneficiaries who receive a government subsidy to offset their drug costs versus those who do not.
The latter group, who can sometimes be on the hook for hundreds of dollars for every prescription they fill, was substantially less likely to actually use their medication as it had been prescribed, even for serious diagnoses like cancer. People receiving subsidies were twice as likely to fill their prescriptions. The study found that 30 percent of prescriptions for anti-cancer drugs and 22 of prescriptions for hepatitis-C treatment were never started.
The problem of drug affordability for Medicare patients has been an ongoing concern. Because of how the program is currently structured, beneficiaries who are enrolled in the traditional Medicare program but do not qualify for subsidies have no upper limit on how much they can be asked to spend on pharmaceuticals in a given year.
As part of the Inflation Reduction Act, Congress is instituting such a cap for the first time, using savings from the new drug pricing controls also included in the law, capping out-of-pocket costs at $2,000 starting in 2025. That is the kind of intervention the Health Affairs authors were calling for when they published the paper. Now we’ll see if that policy change has an effect on seniors actually taking their medicine.
4) Black and Hispanic Americans are less likely to receive CPR in public spaces
One of the experts I asked for input is Harvard Medical School’s Michael Barnett, who publishes his own overview of the year’s best research every year on Twitter. He sent me a few studies, most of which I’ll let him share in his own overview, but one study in particular stuck out, looking at which people are more (or less) likely to get assistance when they have a health emergency in a public setting with other people around.
The paper, published in the New England Journal of Medicine in October by a collection of scholars across the country, examined more than 100,000 incidents of cardiac arrest that occurred outside of the hospital from 2013 to 2019. They focused in particular on whether the person experiencing cardiac arrest in public received CPR from a bystander.
The results were profound: Black and Hispanic people were significantly less likely to be given CPR than a white person, 45 percent versus 60 percent. And this pattern held across neighborhoods of different racial and socioeconomic make-ups. Whether the neighborhood was predominantly white, Black, or Hispanic, up and down the income ladder, in integrated neighborhoods, white people were more likely to receive CPR than someone who is Black and Hispanic.
“Racial and ethnic differences in bystander CPR in public locations raise additional concerns about implicit and explicit biases in layperson response to out-of-hospital cardiac arrests,” the authors wrote.
Racism within the medical system is well established. Black and Hispanic Americans tend to have less access to health care. They tend to have worse experiences with doctors. Clinical trials and other research does not prioritize them. Medical treatments tend to be developed and designed with white people in mind.
But this study would suggest that even the more casual forms of racism and internalized bias can have a real health effect for marginalized Americans.
5) Prices go up after private equity acquires a physician’s practice
Private equity’s deeper investment into US health care is one of the most important ongoing stories in the field right now. The stakes can be life or death, as one paper that I covered last year about mortality rates in nursing homes purchased by private equity firms found. (Of note this year, according to Harvard’s Amitabh Chandra, was another paper that documented the wide disparities in outcomes among nursing homes, even those who are located in the same area.)
A report published by scholars from Johns Hopkins, Harvard, and Oregon Science & Health University in September 2022 in JAMA Health Forum, which Emma Sandoe of North Carolina Medicaid and Duke University shared with me, examined what happened to costs and care utilization when private equity firms had purchased outpatient practices specializing in ophthalmology, dermatology, and gastroenterology, some of their favorite targets.
The study detected several effects: The cost of individual services went up and those practices were seeing more new patients and also charging more time for their existing patients. The amount billed by the private equity-acquired offices per service increased by 20 percent compared to the study’s control group. They saw 38 percent more new patients and there was a 9 percent increase in the number of existing patient visits that were billed as lasting longer than 30 minutes.
On the surface, that could look like partially good news, in spite of the price hikes, with more patients being seen and spending more time with their doctor. But some of the other findings call into question the value of those increases in service volume. In dermatology, the increase in outpatient visits did not correspond to an increase in biopsies ordered. In the gastroenterology practices, there were more visits and scopes but no notable increase in polyp removals. And likewise, at the eye clinics, there was more diagnostic imaging but not any effect on actual cataract removals.
The authors ended their paper with this warning. “Private equity ownership of physician practices has added a distinctly private and market-driven influence to the broader trends in corporate consolidation of physicians by health systems and insurers,” they wrote. “This study contributes evidence for potential overutilization and higher spending on care that will be important for policy makers to monitor.”
----------------------------------------
By: Dylan Scott
Title: 5 studies released in 2022 that might change how you think about health care
Sourced From: www.vox.com/policy-and-politics/2022/12/22/23518648/2022-health-care-research-most-interesting-studies
Published Date: Thu, 22 Dec 2022 15:06:53 +0000






